Why Your Loved One with Borderline Personality Disorder Might Seem Stuck
-
by
Dr Constantina Katsari
- No Comments on Why Your Loved One with Borderline Personality Disorder Might Seem Stuck
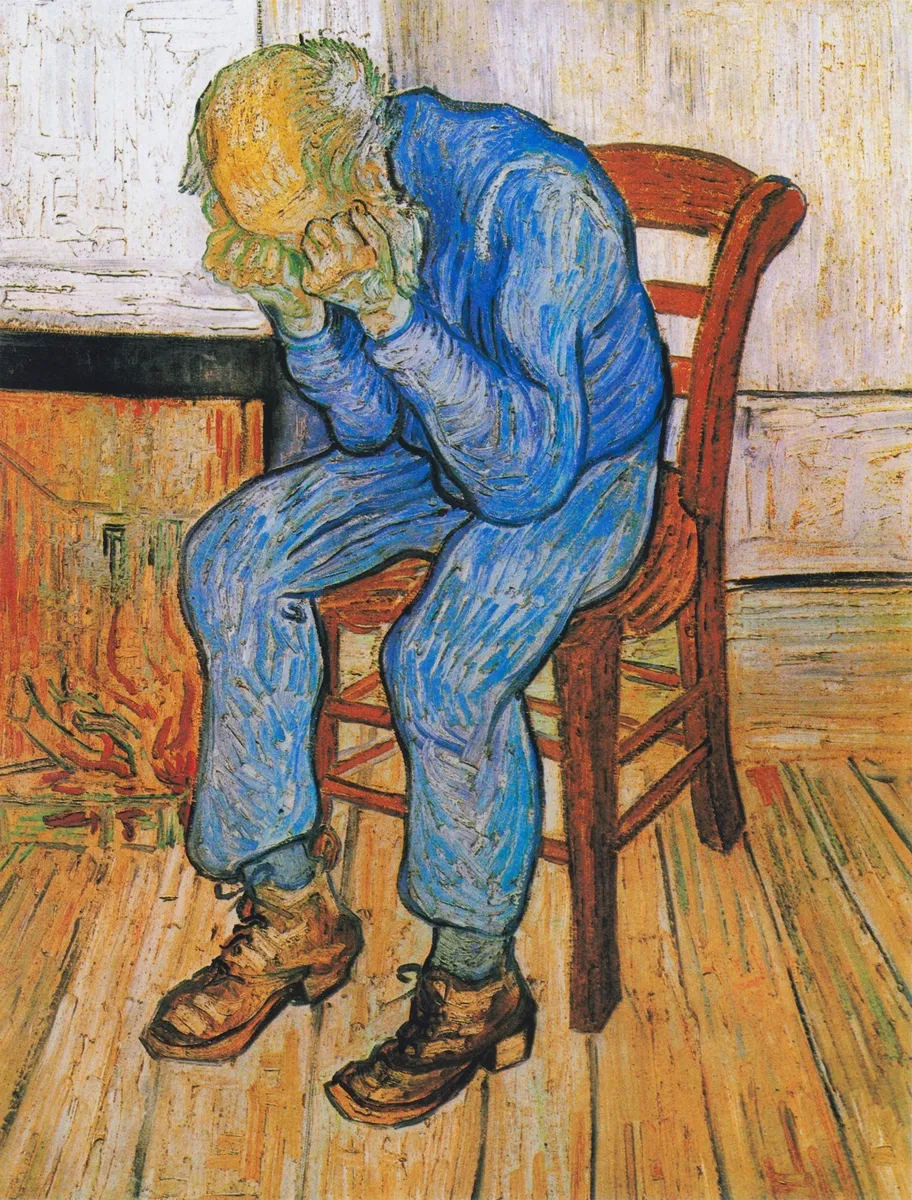
When you care for someone with Borderline Personality Disorder (BPD), the emotional toll is often compounded by confusion. You might ask yourself, “Why do we keep having the same argument?” or “Why can’t they see things differently this time?” It can feel like they’re locked into emotional loops, unable to shift their thinking no matter how much support you offer. A recent study from Cambridge University Press might offer a vital piece of the puzzle and a measure of clarity for those walking this path alongside them.
Published in CNS Spectrums, the study set out to explore whether people with BPD experience specific types of cognitive impairment. The researchers were particularly interested in two functions: cognitive flexibility (the ability to shift mental focus or adapt behaviour in response to change) and executive planning (strategising and problem-solving). These were measured using standardised, computerised tests on two groups: one with BPD and another without.
The results revealed something striking. People with BPD showed a clear difficulty with cognitive flexibility, especially in a task known as “set-shifting.” This task essentially measures how easily someone can switch gears mentally, letting go of one rule or idea and adopting a new one. In contrast, the BPD group did not differ significantly from the control group when it came to planning abilities. In simpler terms: while they can make plans and solve problems just as well as others, they may struggle profoundly when circumstances change or when emotional expectations shift suddenly.
To carers, this might not come as a surprise. How often have you tried to help a loved one see a situation from a new angle, only to watch them revert to a painful narrative that reignites distress? This research helps validate that experience. It shows that the apparent “stuckness” is not just about stubbornness or a lack of insight; it could be rooted in a neurological difficulty with flexibility itself.
Even more compelling was the study’s finding about impulsivity—one of the core features of BPD. Individuals with BPD scored significantly higher on the Barratt Impulsivity Scale than those without the diagnosis. Not only that, but the more impulsive someone was, the more severe their BPD symptoms tended to be. This correlation confirms what many carers already sense: impulsivity isn’t just a feature of the condition; it often fuels its intensity.
Interestingly, while impulsivity was clearly linked to symptom severity, cognitive inflexibility was not. This suggests that inflexibility may be a kind of “baseline” trait in BPD, potentially present even before other symptoms become intense. It could serve as an early vulnerability marker, rather than something that fluctuates with emotional ups and downs. This matters because it shifts how we understand risk. It hints that some of the most difficult behaviours might stem from enduring cognitive patterns, not just from emotional overwhelm in the moment.
At BPD UK, this insight is crucial. Our mission is to equip carers with practical, evidence-informed tools that help them navigate both the crises and the chronic patterns that define life with BPD. Recognising that cognitive flexibility is impaired helps explain why traditional approaches like reasoning, re-framing, or offering perspective may fall short. It’s not that your loved one doesn’t want to understand: they might literally struggle to do so when distressed.
This can also reshape how we approach de-escalation. When someone with BPD is spiralling and seems resistant to help, pushing for a new perspective might actually heighten the distress. Instead, carers might benefit from grounding techniques, validating the current experience, and returning to problem-solving once emotions have stabilised. Understanding that your loved one may need more time and scaffolding to shift mental gears can reduce frustration and prevent emotional burnout.
There are also implications here for early intervention. If cognitive inflexibility is a precursor to symptom severity, it could be targeted in prevention efforts. Digital tools like the BPD Teacher offered by BPD UK are well-positioned to support carers in spotting these patterns early and responding with strategies that support rather than strain the relationship.
It’s important to note that not all areas of cognition were impaired in the BPD group. Planning and problem-solving abilities, as measured by a task similar to the “Tower of Hanoi,” were intact. This nuance matters. It reminds us that people with BPD are not globally impaired; rather, they may have specific difficulties that interact with emotional dysregulation in complex ways. It also underlines the importance of strengths-based approaches. When carers can recognise and build on areas where their loved one is capable, the sense of helplessness on both sides can be reduced.
Still, the research is not without its limitations. The sample size was small, and the study did not account for common BPD comorbidities like depression or ADHD, which can also affect cognition. Nor did it examine how therapy or medication might change these cognitive patterns over time. But as an early investigation, it offers a compelling direction for future studies—especially those taking a longitudinal view.
For carers, the practical takeaway is this: when your loved one seems emotionally stuck, they may also be cognitively stuck. Set-shifting isn’t just a clinical term; it describes the real-world difficulty many people with BPD have in stepping outside their immediate distress or considering alternative interpretations. This isn’t a moral failing. It’s a neurological challenge.
This study is one more step toward an evidence base that includes not just the emotional and relational aspects of BPD, but the cognitive ones too. And for carers who have long sensed that something deeper was at play, it offers both validation and hope.
Read the full article here: Cambridge University Press – Cognition in Adults with Borderline Personality Disorder
https://www.cambridge.org/core/journals/cns-spectrums/article/cognition-in-adults-with-borderline-personality-disorder/C845230A46DA25A76FD110039F813FDF
💬 Caring for someone with BPD?
👉 Book a FREE One2One support session
🧠 Join our FREE webinars and peer groups
📩 To book email us at: info.bpduk@gmail.com
Discover more from BPD UK
Subscribe to get the latest posts sent to your email.